By Theresa Tamkins
This is the second section of a two-part article. Read more about hormones and the risks of heart disease.
Thinking about taking hormones to reduce menopausal symptoms, but concerned about the breast cancer risk? Well, it’s a tricky decision.
Although millions of women were routinely put on hormones during menopause in the past, many stopped taking them in 2002, when one part of the Women’s Health Initiative trial was halted because the hormones didn’t prevent heart disease, as was once hoped, but did increase the risk of breast and ovarian cancer (as well as heart disease and strokes). Read More
Ayurveda and Yoga Blog, Ayurvedic treatments, Natural herbs, herbal remedies, herbal medicine, medicinal herbs, yoga styles, benefits of yoga and herbal supplements for better health and healing.
Showing posts with label breast cancer. Show all posts
Showing posts with label breast cancer. Show all posts
Tuesday, June 03, 2008
Wednesday, February 13, 2008
Precancerous Breast Lesions Cause Unnecessary Worry
(HealthDay News) -- Many women diagnosed with a precancerous breast lesion known as ductal carcinoma in situ (DCIS) are highly anxious about their prognosis, even though they face a low risk of a recurrence or of developing invasive breast cancer, a new study finds.
"Many of these women are living as if they're waiting for the other shoe to drop," said lead researcher Dr. Ann Partridge, an oncologist at the Dana-Farber Cancer Institute and Brigham & Women's Hospital, in Boston.
Her team published the findings Feb. 12 in the online edition of the Journal of the National Cancer Institute.
The study noted that 28 percent of the participants "believed that they had a moderate or greater chance of DCIS spreading to other places in their bodies, despite the fact that metastatic breast cancer actually occurs following a diagnosis of DCIS less than 1 percent of the time."
DCIS involves abnormal cells in the lining of the breast duct that have not spread outside the duct, according to the National Cancer Institute. In 2006, DCIS accounted for more than 20 percent of all diagnoses linked to breast cancer in the United States -- about 62,000 cases, the study reported.
The increasing percentage of DCIS diagnoses over the last 20 years or more has been attributed to improved detection from the increasing use of screening mammography, experts say.
But all too often, women are unnecessarily frightened by a DCIS diagnosis, said the authors of the study, which involved almost 500 women newly diagnosed with DCIS.
"In the complex treatment decision-making process, it is often possible to lose sight of the fact that DCIS poses limited risks to a woman's overall mortality," the study authors noted.
Nevertheless, approximately 38 percent of those surveyed thought they had at least a moderate risk of getting an invasive cancer over the next five years, and 53 percent reported intrusive or avoidant thoughts about DCIS. That number declined to 31 percent 18 months after diagnosis, the researchers said.
Among the 487 study participants who were newly diagnosed with DCIS, 34 percent had undergone a mastectomy, 50 percent had radiation therapy, and 43 percent reported taking tamoxifen to reduce their chances of breast cancer. The type of treatment or combination varied by surgeon, hospital volume and geographic region, the study explained.
"Although decision-making about treatment is complex, there is little doubt that women will be limited in their ability to participate in informed decision-making if they harbor gross misperceptions about the health risks they face," the study authors said. Researchers found a "strong relationship between distress and inaccurate risk perceptions," they added.
One of the difficulties of such measures of anxiety about DCIS is that the study did not determine what these patients had learned from their physicians or from other sources -- such as the Internet -- about DCIS, and how accurate that information was, said Michael Stefanek, vice president of behavioral research for the American Cancer Society.
The choice of treatment depends upon the characteristics of the patient and the lesion, added Partridge, who is also an assistant professor of medicine at Harvard Medical School. The dilemma posed by the prospect of under- or over-treating DCIS is complicated by medicine's current inability to distinguish between "good actors and bad actors" -- lesions that don't recur or go on to become invasive breast cancer and those that do, she added.
Another expert agreed with that assessment.
Everyone would be more comfortable if there wasn't such a "big gray zone" between what is normal tissue and what is invasive cancer, said Dr. H. Gilbert Welch, a professor of medicine at Dartmouth Medical School and an expert on how well health care works for patients. Welch argued that as mammography continues to detect smaller and smaller DCIS lesions, there can be a tendency to over-treat. He recommends that the diagnostic threshold for DCIS be raised to doing biopsies on only lesions that measure 1 centimeter or greater in diameter.
"There is this ironic finding that women with this early precursor lesion may be treated more aggressively than women with invasive breast cancer," he said. "They may have mastectomies instead of just a lumpectomy. At some level we have to say, 'Does this really make sense?'"
Another study in the same issue of JNCI suggests that medical science is winning the war on breast cancer. The research, which involved nearly 5,000 breast cancer patients, was led by the National Cancer Institute of Canada's Clinical Trials Group. A total of 256 of the participants died during the four-year study.
The researchers found that older women who had survived for at least five years after a diagnosis of early stage breast cancer were most likely to die of causes unrelated to their breast malignancy. In fact, 60 percent of these deaths were not caused by breast cancer, the Canadian team found.
More information
For more on DCIS, head to the U.S. National Cancer Institute.
"Many of these women are living as if they're waiting for the other shoe to drop," said lead researcher Dr. Ann Partridge, an oncologist at the Dana-Farber Cancer Institute and Brigham & Women's Hospital, in Boston.
Her team published the findings Feb. 12 in the online edition of the Journal of the National Cancer Institute.
The study noted that 28 percent of the participants "believed that they had a moderate or greater chance of DCIS spreading to other places in their bodies, despite the fact that metastatic breast cancer actually occurs following a diagnosis of DCIS less than 1 percent of the time."
DCIS involves abnormal cells in the lining of the breast duct that have not spread outside the duct, according to the National Cancer Institute. In 2006, DCIS accounted for more than 20 percent of all diagnoses linked to breast cancer in the United States -- about 62,000 cases, the study reported.
The increasing percentage of DCIS diagnoses over the last 20 years or more has been attributed to improved detection from the increasing use of screening mammography, experts say.
But all too often, women are unnecessarily frightened by a DCIS diagnosis, said the authors of the study, which involved almost 500 women newly diagnosed with DCIS.
"In the complex treatment decision-making process, it is often possible to lose sight of the fact that DCIS poses limited risks to a woman's overall mortality," the study authors noted.
Nevertheless, approximately 38 percent of those surveyed thought they had at least a moderate risk of getting an invasive cancer over the next five years, and 53 percent reported intrusive or avoidant thoughts about DCIS. That number declined to 31 percent 18 months after diagnosis, the researchers said.
Among the 487 study participants who were newly diagnosed with DCIS, 34 percent had undergone a mastectomy, 50 percent had radiation therapy, and 43 percent reported taking tamoxifen to reduce their chances of breast cancer. The type of treatment or combination varied by surgeon, hospital volume and geographic region, the study explained.
"Although decision-making about treatment is complex, there is little doubt that women will be limited in their ability to participate in informed decision-making if they harbor gross misperceptions about the health risks they face," the study authors said. Researchers found a "strong relationship between distress and inaccurate risk perceptions," they added.
One of the difficulties of such measures of anxiety about DCIS is that the study did not determine what these patients had learned from their physicians or from other sources -- such as the Internet -- about DCIS, and how accurate that information was, said Michael Stefanek, vice president of behavioral research for the American Cancer Society.
The choice of treatment depends upon the characteristics of the patient and the lesion, added Partridge, who is also an assistant professor of medicine at Harvard Medical School. The dilemma posed by the prospect of under- or over-treating DCIS is complicated by medicine's current inability to distinguish between "good actors and bad actors" -- lesions that don't recur or go on to become invasive breast cancer and those that do, she added.
Another expert agreed with that assessment.
Everyone would be more comfortable if there wasn't such a "big gray zone" between what is normal tissue and what is invasive cancer, said Dr. H. Gilbert Welch, a professor of medicine at Dartmouth Medical School and an expert on how well health care works for patients. Welch argued that as mammography continues to detect smaller and smaller DCIS lesions, there can be a tendency to over-treat. He recommends that the diagnostic threshold for DCIS be raised to doing biopsies on only lesions that measure 1 centimeter or greater in diameter.
"There is this ironic finding that women with this early precursor lesion may be treated more aggressively than women with invasive breast cancer," he said. "They may have mastectomies instead of just a lumpectomy. At some level we have to say, 'Does this really make sense?'"
Another study in the same issue of JNCI suggests that medical science is winning the war on breast cancer. The research, which involved nearly 5,000 breast cancer patients, was led by the National Cancer Institute of Canada's Clinical Trials Group. A total of 256 of the participants died during the four-year study.
The researchers found that older women who had survived for at least five years after a diagnosis of early stage breast cancer were most likely to die of causes unrelated to their breast malignancy. In fact, 60 percent of these deaths were not caused by breast cancer, the Canadian team found.
More information
For more on DCIS, head to the U.S. National Cancer Institute.
Tuesday, September 18, 2007
Gene May Influence Breast Cancer-Estrogen Link
(HealthDay News) -- U.S. researchers say they've found a gene that plays a crucial role in the ability of breast cancer cells to respond to estrogen.
The finding that transcription factor AP2C (TFAP2C) controls multiple pathways of estrogen signaling may lead to improved therapies for hormone-responsive breast cancer and may help explain differences in the effectiveness of current treatments, said a team from the University of Iowa.
The study was published in the Sept. 15 issue of the journal Cancer Research.
"Estrogen binds to estrogen receptors and triggers a cascade of events including gene regulation," study leader Dr. Ronald Weigel, professor and head of surgery at the university's college of medicine, said in a prepared statement.
"We found that elimination of TFAP2C from the cell causes all of those cascades that we associate with estrogen to go away," he said. "The treated cancer cells were not able to respond to estrogen by any normal pathway."
Silencing TFAP2C inhibited tumor growth in mice. It also halted expression of another estrogen receptor called GPR30, found at the cancer cell membrane.
"Targeting this gene may be a better way to develop drugs to treat hormone-responsive breast cancers, because it targets multiple different pathways," Weigel said.
More information
The American Cancer Society has more about breast cancer.
more discussion: Forum
· Addiction Forum · Ask the Doctors Forum · Ayurveda Forum · Ayurvedic & Thai Herbs Forum · Colon Cleansing Forum · Dental Forum · Diabetes Forum · Diet Forum · General Cleansing Forum · Hepatitis A, B. C Forum · Integrated Medicine Forum · Live Blood Analysis Forum · Ozone-Oxygen-Forum · pH - Alkaline - Acidity Forum · Weight Loss Forum
The finding that transcription factor AP2C (TFAP2C) controls multiple pathways of estrogen signaling may lead to improved therapies for hormone-responsive breast cancer and may help explain differences in the effectiveness of current treatments, said a team from the University of Iowa.
The study was published in the Sept. 15 issue of the journal Cancer Research.
"Estrogen binds to estrogen receptors and triggers a cascade of events including gene regulation," study leader Dr. Ronald Weigel, professor and head of surgery at the university's college of medicine, said in a prepared statement.
"We found that elimination of TFAP2C from the cell causes all of those cascades that we associate with estrogen to go away," he said. "The treated cancer cells were not able to respond to estrogen by any normal pathway."
Silencing TFAP2C inhibited tumor growth in mice. It also halted expression of another estrogen receptor called GPR30, found at the cancer cell membrane.
"Targeting this gene may be a better way to develop drugs to treat hormone-responsive breast cancers, because it targets multiple different pathways," Weigel said.
More information
The American Cancer Society has more about breast cancer.
more discussion: Forum
· Addiction Forum · Ask the Doctors Forum · Ayurveda Forum · Ayurvedic & Thai Herbs Forum · Colon Cleansing Forum · Dental Forum · Diabetes Forum · Diet Forum · General Cleansing Forum · Hepatitis A, B. C Forum · Integrated Medicine Forum · Live Blood Analysis Forum · Ozone-Oxygen-Forum · pH - Alkaline - Acidity Forum · Weight Loss Forum
Labels:
Ayurveda,
Ayurveda Herbs,
Ayurveda therapy,
ayurvedic,
breast cancer,
diabetes,
diet,
help,
herbs,
weight loss
Saturday, September 15, 2007
Tomato Diet Can't Guarantee Prostate Health: Study
(HealthDay News) -- Men who've been adding vitamin E or the tomato nutrient lycopene to their diets to cut their risk of prostate cancer may need to think again.
According to a new study, neither carotenoids (such as lycopene), retinol, nor tocopherols (forms of vitamin E) appear to reduce the odds of prostate malignancy -- findings that are in line with two other recent publications.
"Our overall findings are null," said lead researcher Timothy Key, deputy director of the Cancer Research UK Epidemiology Unit at the University of Oxford, U.K.
"This large study does not support the hypothesis that consuming large amounts of these nutrients will reduce prostate cancer," he added. "That is disappointing, but that is the overall message."
The findings are published in the September issue of the American Journal of Clinical Nutrition.
His team examined the effect of the blood levels of 10 micronutrients on the risk of developing prostate cancer for almost 2,000 males from eight European countries.
The research, which the authors call "the largest prospective study to date of plasma carotenoids, retinol, tocopherols, and prostate cancer risk," was part of the EPIC (European Prospective Investigation into Cancer and Nutrition) study, which includes more than half a million men and women.
The authors did find evidence to suggest that, once a cancer forms, high levels of lycopene (or of carotenoids in general, including lycopene) may reduce by about 60 percent the risk of the tumor progressing to an advanced-stage prostate cancer. Carotenoids appeared to have no effect on the rate of localized, earlier-stage disease, however.
According to Dr. Peter Scardino, head of the Prostate Cancer Program at Memorial Sloan-Kettering Cancer Center in New York City, prostate cancer is the most common cancer in men in the developed world. A Western male, he said, has about a 42 percent risk of developing cancerous cells in his prostate over his lifetime, a 16 percent risk of being diagnosed with the disease, and about a three percent risk of dying as a result. In other words, nearly one-quarter of Western males have a subclinical form of prostate cancer, which will never progress to more advanced disease.
Stopping progression is crucial. According to Scardino, for those whose disease does progress, the risk of death is much higher -- nearly 50 percent.
"I think it's an important study," Scardino said. That lycopene and bulk carotenoids reduced the risk of progressing to advanced disease without impacting the risk of developing prostate cancer overall, he said, "suggests maybe these micronutrients are not as important in [stopping] carcinogenesis as they are in [slowing] progression of a very small early tumor to one that becomes invasive and larger and develops the ability to metastasize."
"The study provides supportive evidence that lycopene and the carotenoids may have an effect on delaying the progression of prostate cancer, so, from that point of view, it is an interesting study," Scardino added.
But Alan Kristal, associate head of the Cancer Prevention Program at the Fred Hutchinson Cancer Research Center in Seattle, remained more skeptical. Though he called the study "well-executed," Kristal noted, for instance, that the authors were unable to control for prostate-specific antigen (PSA) testing among the men. These blood tests often detect clinically irrelevant tumors, he explained.
"You can never do an observational study of prostate cancer without rigorously controlling for whether or not the person got PSA screening," Kristal said. "The more times you take the test, the more likely you are to get the disease."
He also noted that the finding for lycopene contradicts a report published in May in Cancer Epidemiology Biomarkers and Prevention. That study did account for PSA testing, and it found no effect of lycopene whatsoever on prostate cancer risk -- including the risk of advanced disease.
"To my mind, that study is definitive," said Kristal. "It's a big study, extremely well executed, properly analyzed, and not biased by PSA screening."
A review of lycopene's effect on cancer by the U.S. Food and Drug Administration, published in July in the Journal of the National Cancer Institute, likewise found "no credible evidence to support an association between lycopene intake and a reduced risk of prostate, lung, colorectal, gastric, breast, ovarian, endometrial, or pancreatic cancer and very limited evidence to support an association between tomato consumption and reduced risks of prostate, ovarian, gastric, and pancreatic cancers," according to that study's authors.
So, with tomatoes, ketchup and pizza sauce crossed off the list of prostate-protecting foods, Key and others continue the search. Kristal, for instance, is on the executive committee of a randomized trial examining the effects of selenium and/or vitamin E on prostate cancer risk in 35,000 men. Results are expected in 2012, he said.
Said Key, "I am optimistic we will find something. This paper is an important piece of work, but it doesn't look like this is the answer."
More information
For more on vitamins and cancer, visit the American Cancer Society.
more discussion: Forum
· Addiction Forum · Ask the Doctors Forum · Ayurveda Forum · Ayurvedic & Thai Herbs Forum · Colon Cleansing Forum · Dental Forum · Diabetes Forum · Diet Forum · General Cleansing Forum · Hepatitis A, B. C Forum · Integrated Medicine Forum · Live Blood Analysis Forum · Ozone-Oxygen-Forum · pH - Alkaline - Acidity Forum · Weight Loss Forum
According to a new study, neither carotenoids (such as lycopene), retinol, nor tocopherols (forms of vitamin E) appear to reduce the odds of prostate malignancy -- findings that are in line with two other recent publications.
"Our overall findings are null," said lead researcher Timothy Key, deputy director of the Cancer Research UK Epidemiology Unit at the University of Oxford, U.K.
"This large study does not support the hypothesis that consuming large amounts of these nutrients will reduce prostate cancer," he added. "That is disappointing, but that is the overall message."
The findings are published in the September issue of the American Journal of Clinical Nutrition.
His team examined the effect of the blood levels of 10 micronutrients on the risk of developing prostate cancer for almost 2,000 males from eight European countries.
The research, which the authors call "the largest prospective study to date of plasma carotenoids, retinol, tocopherols, and prostate cancer risk," was part of the EPIC (European Prospective Investigation into Cancer and Nutrition) study, which includes more than half a million men and women.
The authors did find evidence to suggest that, once a cancer forms, high levels of lycopene (or of carotenoids in general, including lycopene) may reduce by about 60 percent the risk of the tumor progressing to an advanced-stage prostate cancer. Carotenoids appeared to have no effect on the rate of localized, earlier-stage disease, however.
According to Dr. Peter Scardino, head of the Prostate Cancer Program at Memorial Sloan-Kettering Cancer Center in New York City, prostate cancer is the most common cancer in men in the developed world. A Western male, he said, has about a 42 percent risk of developing cancerous cells in his prostate over his lifetime, a 16 percent risk of being diagnosed with the disease, and about a three percent risk of dying as a result. In other words, nearly one-quarter of Western males have a subclinical form of prostate cancer, which will never progress to more advanced disease.
Stopping progression is crucial. According to Scardino, for those whose disease does progress, the risk of death is much higher -- nearly 50 percent.
"I think it's an important study," Scardino said. That lycopene and bulk carotenoids reduced the risk of progressing to advanced disease without impacting the risk of developing prostate cancer overall, he said, "suggests maybe these micronutrients are not as important in [stopping] carcinogenesis as they are in [slowing] progression of a very small early tumor to one that becomes invasive and larger and develops the ability to metastasize."
"The study provides supportive evidence that lycopene and the carotenoids may have an effect on delaying the progression of prostate cancer, so, from that point of view, it is an interesting study," Scardino added.
But Alan Kristal, associate head of the Cancer Prevention Program at the Fred Hutchinson Cancer Research Center in Seattle, remained more skeptical. Though he called the study "well-executed," Kristal noted, for instance, that the authors were unable to control for prostate-specific antigen (PSA) testing among the men. These blood tests often detect clinically irrelevant tumors, he explained.
"You can never do an observational study of prostate cancer without rigorously controlling for whether or not the person got PSA screening," Kristal said. "The more times you take the test, the more likely you are to get the disease."
He also noted that the finding for lycopene contradicts a report published in May in Cancer Epidemiology Biomarkers and Prevention. That study did account for PSA testing, and it found no effect of lycopene whatsoever on prostate cancer risk -- including the risk of advanced disease.
"To my mind, that study is definitive," said Kristal. "It's a big study, extremely well executed, properly analyzed, and not biased by PSA screening."
A review of lycopene's effect on cancer by the U.S. Food and Drug Administration, published in July in the Journal of the National Cancer Institute, likewise found "no credible evidence to support an association between lycopene intake and a reduced risk of prostate, lung, colorectal, gastric, breast, ovarian, endometrial, or pancreatic cancer and very limited evidence to support an association between tomato consumption and reduced risks of prostate, ovarian, gastric, and pancreatic cancers," according to that study's authors.
So, with tomatoes, ketchup and pizza sauce crossed off the list of prostate-protecting foods, Key and others continue the search. Kristal, for instance, is on the executive committee of a randomized trial examining the effects of selenium and/or vitamin E on prostate cancer risk in 35,000 men. Results are expected in 2012, he said.
Said Key, "I am optimistic we will find something. This paper is an important piece of work, but it doesn't look like this is the answer."
More information
For more on vitamins and cancer, visit the American Cancer Society.
more discussion: Forum
· Addiction Forum · Ask the Doctors Forum · Ayurveda Forum · Ayurvedic & Thai Herbs Forum · Colon Cleansing Forum · Dental Forum · Diabetes Forum · Diet Forum · General Cleansing Forum · Hepatitis A, B. C Forum · Integrated Medicine Forum · Live Blood Analysis Forum · Ozone-Oxygen-Forum · pH - Alkaline - Acidity Forum · Weight Loss Forum
Labels:
Ayurveda,
Ayurveda Herbs,
Ayurveda therapy,
ayurvedic,
breast cancer,
diabetes,
diet,
herbs,
weight loss
Wednesday, December 13, 2006
Exercise Cuts Breast Cancer Risk
(HealthDay News) -- Postmenopausal women who engage in more vigorous physical activity seem to have a lower risk of breast cancer.
The beneficial effect was most pronounced for estrogen receptor positive/progesterone receptor negative tumors, which are generally more aggressive.
"It seems like another confirmation to the fact that exercise will help reduce the risk of breast carcinoma and may play some other interesting roles in addition to effects on cardiovascular health," said Dr. Jay Brooks, chairman of hematology/oncology at Ochsner Health System in Baton Rouge, La.
While overweight and obesity are risk factors for breast cancer, the findings also suggest that additional mechanisms may be involved in promoting the growth of tumors.
The association between exercise and a reduced risk of breast cancer is not a new one. Previous studies have shown that physical activity can reduce the risk for the disease among women of all ages.
But because breast cancer is such a varied disease, there may be different risk factors, depending on different tumor characteristics, including estrogen receptor (ER) and progesterone receptor (PR) status. Receptor status refers to whether these hormones bind to the surface of the tumor.
Only three small studies have looked at the association between physical activity and postmenopausal breast cancer defined by receptor status, the study authors said.
The new study, called the Iowa Women's Health Study, is the largest study to cross-classify estrogen receptor (ER) and progesterone receptor (PR) status, said Dr. James Cerhan, senior author of the study and professor of epidemiology at the Mayo Clinic College of Medicine in Rochester, Minn. The findings are published in the Dec. 11/25 issue of Archives of Internal Medicine.
Cerhan and his colleagues looked at 41,836 postmenopausal women who were between the ages of 55 and 69 in 1986. The participants filled out a 16-page questionnaire at the beginning of the study about their recreational physical activity and then were monitored for 18 years.
Women who engaged in high levels of physical activity had a 14 percent lower risk of breast cancer than those who participated in low levels of activity. After the researchers adjusted for body mass index (BMI, a ratio of weight to height), they found that women with high physical activity levels had a 9 percent lower risk of breast cancer.
"Physical activity protected against breast cancer, but when we adjusted for BMI, it weakened the association," Cerhan explained.
This would imply that something in addition to exercise contributed to the protective effect.
The findings were even more striking when hormone receptor status was taken into account. Women with high physical activity levels had a 33 percent lower risk of developing estrogen receptor-positive tumors.
High levels of physical activity included vigorous exercise such as jogging, swimming or racket sports two or more times a week or moderate activity such as bowling, golf, gardening or walking more than four times a week. Medium physical activity was vigorous activity once a week or moderate activity one to four times a week.
Being overweight is a well-known risk factor for breast cancer, as body fat produces estrogen that signals some tumors to grow.
"This is another reason to be physically active. But I think much of the information is for medical scientists trying to think about the mechanisms of breast cancer," Cerhan said.
More information
To learn more about breast cancer, visit the American Cancer Society.
The beneficial effect was most pronounced for estrogen receptor positive/progesterone receptor negative tumors, which are generally more aggressive.
"It seems like another confirmation to the fact that exercise will help reduce the risk of breast carcinoma and may play some other interesting roles in addition to effects on cardiovascular health," said Dr. Jay Brooks, chairman of hematology/oncology at Ochsner Health System in Baton Rouge, La.
While overweight and obesity are risk factors for breast cancer, the findings also suggest that additional mechanisms may be involved in promoting the growth of tumors.
The association between exercise and a reduced risk of breast cancer is not a new one. Previous studies have shown that physical activity can reduce the risk for the disease among women of all ages.
But because breast cancer is such a varied disease, there may be different risk factors, depending on different tumor characteristics, including estrogen receptor (ER) and progesterone receptor (PR) status. Receptor status refers to whether these hormones bind to the surface of the tumor.
Only three small studies have looked at the association between physical activity and postmenopausal breast cancer defined by receptor status, the study authors said.
The new study, called the Iowa Women's Health Study, is the largest study to cross-classify estrogen receptor (ER) and progesterone receptor (PR) status, said Dr. James Cerhan, senior author of the study and professor of epidemiology at the Mayo Clinic College of Medicine in Rochester, Minn. The findings are published in the Dec. 11/25 issue of Archives of Internal Medicine.
Cerhan and his colleagues looked at 41,836 postmenopausal women who were between the ages of 55 and 69 in 1986. The participants filled out a 16-page questionnaire at the beginning of the study about their recreational physical activity and then were monitored for 18 years.
Women who engaged in high levels of physical activity had a 14 percent lower risk of breast cancer than those who participated in low levels of activity. After the researchers adjusted for body mass index (BMI, a ratio of weight to height), they found that women with high physical activity levels had a 9 percent lower risk of breast cancer.
"Physical activity protected against breast cancer, but when we adjusted for BMI, it weakened the association," Cerhan explained.
This would imply that something in addition to exercise contributed to the protective effect.
The findings were even more striking when hormone receptor status was taken into account. Women with high physical activity levels had a 33 percent lower risk of developing estrogen receptor-positive tumors.
High levels of physical activity included vigorous exercise such as jogging, swimming or racket sports two or more times a week or moderate activity such as bowling, golf, gardening or walking more than four times a week. Medium physical activity was vigorous activity once a week or moderate activity one to four times a week.
Being overweight is a well-known risk factor for breast cancer, as body fat produces estrogen that signals some tumors to grow.
"This is another reason to be physically active. But I think much of the information is for medical scientists trying to think about the mechanisms of breast cancer," Cerhan said.
More information
To learn more about breast cancer, visit the American Cancer Society.
Thursday, October 19, 2006
Does Breastfeeding Prevent Breast Cancer?
Does Breastfeeding Prevent Breast Cancer?
Is it true that the longer your breastfeed your babies, the lower your risk of breast cancer?
Yes, breastfeeding does appear to protect against breast cancer, probably by affecting levels of estrogen in a woman's body. Results of a study published in the July 20, 2002, issue of The Lancet showed that the more babies a woman has and the longer she nurses them, the lower her risk of breast cancer. The researchers reviewed 47 reports of studies in 30 countries that contained information about 50,000 women with breast cancer and almost 97,000 women who didn’t develop breast cancer.
The study reported that women in developed countries who had never had breast cancer breastfed their babies for an average of three months per child. In developing countries in Africa and Asia, women breastfed each of their babies for an average of 30 months.
We’ve known for a long time that the more often a woman gives birth, the lower her risk of breast cancer. This study showed that each birth reduced a woman’s risk by seven percent. Among those who breastfed their children (compared to those who had children but didn’t breastfeed) the breast cancer risk declined by about four percent for each year of breastfeeding.
The researchers also looked at how breastfeeding and pregnancy would affect the risk of breast cancer if women in developed countries had the same number of babies and breastfed them as long as women in developing countries. They found that the risk would be cut by more than half and that almost two thirds of the reduced risk was due to breastfeeding alone.
The Collaborative Group on Hormonal Factors in Breast Cancer, which conducted the study, concluded that the short duration of breastfeeding among women in developed countries makes a major contribution to the higher incidence of breast cancer in these areas. The researchers said their findings suggest that if women had an average of two-and-one-half children and breastfed each one an extra six months, five percent of breast cancers would be prevented each year; if they breastfed each child for an additional 12 months, 11 percent of cancers would be prevented each year.
That’s a powerful argument for breastfeeding. We know that breastfeeding is good for babies. This study proved that it can be very good for mothers, too.
Andrew Weil, M.D.
Is it true that the longer your breastfeed your babies, the lower your risk of breast cancer?
Yes, breastfeeding does appear to protect against breast cancer, probably by affecting levels of estrogen in a woman's body. Results of a study published in the July 20, 2002, issue of The Lancet showed that the more babies a woman has and the longer she nurses them, the lower her risk of breast cancer. The researchers reviewed 47 reports of studies in 30 countries that contained information about 50,000 women with breast cancer and almost 97,000 women who didn’t develop breast cancer.
The study reported that women in developed countries who had never had breast cancer breastfed their babies for an average of three months per child. In developing countries in Africa and Asia, women breastfed each of their babies for an average of 30 months.
We’ve known for a long time that the more often a woman gives birth, the lower her risk of breast cancer. This study showed that each birth reduced a woman’s risk by seven percent. Among those who breastfed their children (compared to those who had children but didn’t breastfeed) the breast cancer risk declined by about four percent for each year of breastfeeding.
The researchers also looked at how breastfeeding and pregnancy would affect the risk of breast cancer if women in developed countries had the same number of babies and breastfed them as long as women in developing countries. They found that the risk would be cut by more than half and that almost two thirds of the reduced risk was due to breastfeeding alone.
The Collaborative Group on Hormonal Factors in Breast Cancer, which conducted the study, concluded that the short duration of breastfeeding among women in developed countries makes a major contribution to the higher incidence of breast cancer in these areas. The researchers said their findings suggest that if women had an average of two-and-one-half children and breastfed each one an extra six months, five percent of breast cancers would be prevented each year; if they breastfed each child for an additional 12 months, 11 percent of cancers would be prevented each year.
That’s a powerful argument for breastfeeding. We know that breastfeeding is good for babies. This study proved that it can be very good for mothers, too.
Andrew Weil, M.D.
Wrong Treatment for Breast Cancer?
Wrong Treatment for Breast Cancer?
I'm recovering from breast cancer. I had a lumpectomy plus radiation, and I've been told that the outlook for a cure is excellent. However, I've just heard that radiation is no longer considered necessary. Did I have needless treatment?
Two studies published in the Sept. 2, 2004, issue of the New England Journal of Medicine suggest that radiation treatment is not necessary for older women who have small tumors and take the drug tamoxifen after surgery. Tamoxifen blocks the hormone estrogen from affecting breast cancer cells. Most cases of breast cancer are "estrogen-receptor positive" meaning that the disease is fed by estrogen.
If you're under 70, the evidence still shows that it is best to have radiation after surgery for early breast cancer. However, treatment always has to be individualized based on the specifics of a woman's case, including the size of the tumor. One of the studies also suggested that some women over 60 with very small tumors probably can forego radiation treatment as long as they take tamoxifen.
The first study, from Boston's Massachusetts General Hospital, included 636 women over the age of 70. The researchers found that only one percent of those who took tamoxifen and had radiation treatment after surgery had a recurrence of cancer in the same breast in the approximately five years after they were treated. Among those who took tamoxifen but didn't have radiation, only four percent had a cancer recurrence.
The other study, from Canada, included 769 women over the age of 50. It found that 0.6 percent of those who had radiation and took tamoxifen had a recurrence, compared to 7.7 percent of those who didn't have radiation. However, among the women 60 and older, only 1.2 percent of those who didn't have radiation developed recurrences. This study included women with larger tumors as well as those whose breast cancer was estrogen-receptor negative, a more aggressive type of the disease. Typically, radiation treatment for women with breast cancer means 16 sessions over three weeks. Side effects can include burning of the skin, redness, swelling and fatigue.
As far as the care you received, I wouldn't worry about being treated unnecessarily. If you're under 60, there's little argument that the best approach is radiation plus tamoxifen. Whatever your age, be thankful that the disease was caught early.
Andrew Weil, M.D.
I'm recovering from breast cancer. I had a lumpectomy plus radiation, and I've been told that the outlook for a cure is excellent. However, I've just heard that radiation is no longer considered necessary. Did I have needless treatment?
Two studies published in the Sept. 2, 2004, issue of the New England Journal of Medicine suggest that radiation treatment is not necessary for older women who have small tumors and take the drug tamoxifen after surgery. Tamoxifen blocks the hormone estrogen from affecting breast cancer cells. Most cases of breast cancer are "estrogen-receptor positive" meaning that the disease is fed by estrogen.
If you're under 70, the evidence still shows that it is best to have radiation after surgery for early breast cancer. However, treatment always has to be individualized based on the specifics of a woman's case, including the size of the tumor. One of the studies also suggested that some women over 60 with very small tumors probably can forego radiation treatment as long as they take tamoxifen.
The first study, from Boston's Massachusetts General Hospital, included 636 women over the age of 70. The researchers found that only one percent of those who took tamoxifen and had radiation treatment after surgery had a recurrence of cancer in the same breast in the approximately five years after they were treated. Among those who took tamoxifen but didn't have radiation, only four percent had a cancer recurrence.
The other study, from Canada, included 769 women over the age of 50. It found that 0.6 percent of those who had radiation and took tamoxifen had a recurrence, compared to 7.7 percent of those who didn't have radiation. However, among the women 60 and older, only 1.2 percent of those who didn't have radiation developed recurrences. This study included women with larger tumors as well as those whose breast cancer was estrogen-receptor negative, a more aggressive type of the disease. Typically, radiation treatment for women with breast cancer means 16 sessions over three weeks. Side effects can include burning of the skin, redness, swelling and fatigue.
As far as the care you received, I wouldn't worry about being treated unnecessarily. If you're under 60, there's little argument that the best approach is radiation plus tamoxifen. Whatever your age, be thankful that the disease was caught early.
Andrew Weil, M.D.
Does Drinking Milk Lead to Breast Cancer?
Does Drinking Milk Lead to Breast Cancer?
Is there any correlation between milk-drinking and breast cancer? I've been reading vegetarian Web sites that say there could be a link.
Evidence connecting milk consumption to breast cancer is contradictory, but results of a recent study from Denmark suggest that it may play a role in the increasing incidence of the disease during the past 50 years. In a study involving more than 117,000 women, researchers from the Statens Serum Institute found that height is a risk factor for breast cancer, particularly when it stems from a growth spurt between the ages of eight and 14. In Japan, an increase in women's average heights over the last 50 years may be related to milk consumption. During that time breast cancer incidence doubled from 40 to 80 cases per 100,000 women. The findings were published in the October 14, 2004, issue of the New England Journal of Medicine.
Commenting on the results in the same issue, two experts from Harvard Medical School noted that milk consumption increases circulating levels of insulin-like growth factor 1, a growth hormone associated with higher stature. It isn't known yet exactly how this might contribute to childhood growth and breast cancer risk. But if milk drinking is to blame for the increased incidence of breast cancer, the amount consumed during childhood could be the key, not the amount adult women are drinking today.

To confuse matters, an earlier study had suggested that the vitamin D and calcium women get by consuming low-fat dairy products, including skim or low-fat milk lower the risk of breast cancer before menopause but not afterward. These findings came from data drawn from the famed Nurses Health Study, which began in 1976 and includes more than 120,000 nurses in 11 states. In 2002 Harvard researchers published an analysis of information from more than 88,600 of the women showing that consumption of dairy products - either before or after menopause - had no effect one way or the other on the breast cancer risk among postmenopausal women. The study was published in the September 4, 2002, issue of the Journal of the National Cancer Institute.
Another study, from Norway, published in 2001 also suggested that milk consumption was protective. Data from more than 48,000 premenopausal women researchers showed that childhood milk consumption (regardless of the type of milk and its fat content) was associated with a lower breast cancer risk among women aged 34 to 39 but not among women in their forties. Adult milk consumption also seemed to lower the risk. Among women who drank more than three glasses of milk per day, risk was lowered by about half. The study was published in the Sept. 15, 2001 issue of the International Journal of Cancer.
I recommend against using cow's milk and products made from milk if you have a personal or family history of eczema, asthma, bronchitis, sinusitis, or autoimmunity. If you do drink milk, I urge you to buy only organic brands without the residues of antibiotics and hormones found in conventional brands. In my opinion, those hormone residues may be the factor responsible for increased risks of cancer, especially hormonally driven cancers.
Andrew Weil, M.D.
Is there any correlation between milk-drinking and breast cancer? I've been reading vegetarian Web sites that say there could be a link.
Evidence connecting milk consumption to breast cancer is contradictory, but results of a recent study from Denmark suggest that it may play a role in the increasing incidence of the disease during the past 50 years. In a study involving more than 117,000 women, researchers from the Statens Serum Institute found that height is a risk factor for breast cancer, particularly when it stems from a growth spurt between the ages of eight and 14. In Japan, an increase in women's average heights over the last 50 years may be related to milk consumption. During that time breast cancer incidence doubled from 40 to 80 cases per 100,000 women. The findings were published in the October 14, 2004, issue of the New England Journal of Medicine.
Commenting on the results in the same issue, two experts from Harvard Medical School noted that milk consumption increases circulating levels of insulin-like growth factor 1, a growth hormone associated with higher stature. It isn't known yet exactly how this might contribute to childhood growth and breast cancer risk. But if milk drinking is to blame for the increased incidence of breast cancer, the amount consumed during childhood could be the key, not the amount adult women are drinking today.

To confuse matters, an earlier study had suggested that the vitamin D and calcium women get by consuming low-fat dairy products, including skim or low-fat milk lower the risk of breast cancer before menopause but not afterward. These findings came from data drawn from the famed Nurses Health Study, which began in 1976 and includes more than 120,000 nurses in 11 states. In 2002 Harvard researchers published an analysis of information from more than 88,600 of the women showing that consumption of dairy products - either before or after menopause - had no effect one way or the other on the breast cancer risk among postmenopausal women. The study was published in the September 4, 2002, issue of the Journal of the National Cancer Institute.
Another study, from Norway, published in 2001 also suggested that milk consumption was protective. Data from more than 48,000 premenopausal women researchers showed that childhood milk consumption (regardless of the type of milk and its fat content) was associated with a lower breast cancer risk among women aged 34 to 39 but not among women in their forties. Adult milk consumption also seemed to lower the risk. Among women who drank more than three glasses of milk per day, risk was lowered by about half. The study was published in the Sept. 15, 2001 issue of the International Journal of Cancer.
I recommend against using cow's milk and products made from milk if you have a personal or family history of eczema, asthma, bronchitis, sinusitis, or autoimmunity. If you do drink milk, I urge you to buy only organic brands without the residues of antibiotics and hormones found in conventional brands. In my opinion, those hormone residues may be the factor responsible for increased risks of cancer, especially hormonally driven cancers.
Andrew Weil, M.D.
Do Diet and Exercise Prevent Breast Cancer Recurrence?
Do Diet and Exercise Prevent Breast Cancer Recurrence?I'm a breast cancer survivor. I read that a low-fat diet reduces the risk of a recurrence. I was treated three years ago. Do you think that the diet can help me? What about exercise?
A low-fat diet certainly couldn't hurt, and a new study shows that getting regular exercise can help a lot. The news that a low-fat diet reduces the rate of breast cancer recurrence comes from a study reported recently at a meeting of the American Society of Clinical Oncology. It is the first study to demonstrate that diet directly affects breast cancer.
Of the 975 women who followed a low-fat diet, 96 (or 9.8 percent) had recurrences of their breast cancer over a five-year period compared to 181 (or 12.4 percent) of the 1,462 women who stayed on their usual diet. All of the women had undergone surgery (lumpectomy or mastectomy) followed by radiation and then hormonal therapy or chemotherapy when indicated. The women were assigned to the low-fat diet at random.
Although researchers said that more study is needed before recommending low- fat diets to all breast cancer patients, there is no reason not to cut your fat intake. Doing so will also reduce your risk of heart disease, and, if necessary, help you lose weight. (Simply losing weight after breast cancer treatment has been shown to reduce the risk of recurrence.) Interestingly, the women whose recurrence rate was lowest on the low-fat diet were those whose breast cancers were estrogen receptor negative, meaning that they didn't depend on estrogen to grow.
Researchers from the University of California at Los Angeles who conducted the low-fat diet study limited the women to an average of 33.3 grams of fat per day, a little more than one ounce of fat, compared to the 51.2 grams of fat per day consumed by the women who followed their usual diets. I still recommend that however much fat you eat, you try to choose the right kinds - monounsaturated fat found in olive oil, nuts and avocados, and omega-3-rich fat from cold water fish, flax (try freshly ground flaxseeds), and walnuts. Also choose low-glycemic carbohydrates and lean sources of protein.
As far as exercise is concerned, a study published in the May 25, 2005 issue of the Journal of the American Medical Association found that it improved survival among women who have had breast cancer even if they walked as little as an hour a week. The authors noted that after a breast cancer diagnosis, women decrease their levels of physical activity by two hours a week and that even greater decreases have been seen among obese women.
The researchers found that the risk of death from breast cancer for women who have had breast cancer and walk at least an hour a week at a pace of two to 2.9 miles per hour was 20 percent lower than those who got less exercise or none at all. Those who walked three to five hours a week had a risk of death 50 percent lower than those who got little or no exercise. Those who got even more exercise also reduced their risk of death but, unaccountably, by somewhat less than 50 percent.
These findings make a lot of sense when you consider that physical activity affects circulating hormones. Lower estrogen levels among the physically active women might explain their improved survival, according to the study authors. (They noted that the benefit of physical activity was particularly apparent among women whose breast tumors were fed by estrogen.) Overall, the study makes a strong case for continuing to get regular exercise after a breast cancer diagnosis.
Andrew Weil, M.D.
A low-fat diet certainly couldn't hurt, and a new study shows that getting regular exercise can help a lot. The news that a low-fat diet reduces the rate of breast cancer recurrence comes from a study reported recently at a meeting of the American Society of Clinical Oncology. It is the first study to demonstrate that diet directly affects breast cancer.
Of the 975 women who followed a low-fat diet, 96 (or 9.8 percent) had recurrences of their breast cancer over a five-year period compared to 181 (or 12.4 percent) of the 1,462 women who stayed on their usual diet. All of the women had undergone surgery (lumpectomy or mastectomy) followed by radiation and then hormonal therapy or chemotherapy when indicated. The women were assigned to the low-fat diet at random.
Although researchers said that more study is needed before recommending low- fat diets to all breast cancer patients, there is no reason not to cut your fat intake. Doing so will also reduce your risk of heart disease, and, if necessary, help you lose weight. (Simply losing weight after breast cancer treatment has been shown to reduce the risk of recurrence.) Interestingly, the women whose recurrence rate was lowest on the low-fat diet were those whose breast cancers were estrogen receptor negative, meaning that they didn't depend on estrogen to grow.
Researchers from the University of California at Los Angeles who conducted the low-fat diet study limited the women to an average of 33.3 grams of fat per day, a little more than one ounce of fat, compared to the 51.2 grams of fat per day consumed by the women who followed their usual diets. I still recommend that however much fat you eat, you try to choose the right kinds - monounsaturated fat found in olive oil, nuts and avocados, and omega-3-rich fat from cold water fish, flax (try freshly ground flaxseeds), and walnuts. Also choose low-glycemic carbohydrates and lean sources of protein.
As far as exercise is concerned, a study published in the May 25, 2005 issue of the Journal of the American Medical Association found that it improved survival among women who have had breast cancer even if they walked as little as an hour a week. The authors noted that after a breast cancer diagnosis, women decrease their levels of physical activity by two hours a week and that even greater decreases have been seen among obese women.
The researchers found that the risk of death from breast cancer for women who have had breast cancer and walk at least an hour a week at a pace of two to 2.9 miles per hour was 20 percent lower than those who got less exercise or none at all. Those who walked three to five hours a week had a risk of death 50 percent lower than those who got little or no exercise. Those who got even more exercise also reduced their risk of death but, unaccountably, by somewhat less than 50 percent.
These findings make a lot of sense when you consider that physical activity affects circulating hormones. Lower estrogen levels among the physically active women might explain their improved survival, according to the study authors. (They noted that the benefit of physical activity was particularly apparent among women whose breast tumors were fed by estrogen.) Overall, the study makes a strong case for continuing to get regular exercise after a breast cancer diagnosis.
Andrew Weil, M.D.
Wednesday, October 04, 2006
Menopause Relief
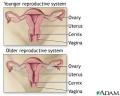 Ayurveda offers a new line of products for menopausal symptoms that are not only effective but safe. When research on hormone-replacement therapy (HRT) was suddenly discontinued by a federally-funded research program this summer, it made headlines.
Ayurveda offers a new line of products for menopausal symptoms that are not only effective but safe. When research on hormone-replacement therapy (HRT) was suddenly discontinued by a federally-funded research program this summer, it made headlines.A combination of artificial estrogen and progestin, HRT has been used by millions of women as a solution to a wide range of menopausal problems from hot flashes to wrinkle-free skin.
The reason for discontinuing HRT research: despite the fact that HRT has been promoted by doctors and researchers as a way to protect women against heart disease for the past thirty years, the study proved that the opposite is true.
Long-term use of HRT actually increases the risk of cardiovascular disease, stroke and clotting, and thus the 16,000 subjects involved in HRT research were at too high a risk to continue. In addition, the study definitively proved what was already indicated in 30 previous studies--that HRT also increases the risk of breast cancer.
The HRT study was conducted by the Women's Health Initiative (WHI), one of the largest research programs ever undertaken, involving over 160,000 women subjects. The WHI was begun in 1991 by the National Institutes of Health and is considered the definitive word on women's health by most doctors due to its rigorous design.
So what is a woman to do? Millions of women now feel abandoned, adrift in a sea of symptoms without relief. Many are turning to Maharishi Ayurveda for help.
Maharishi Ayurveda Products has recently developed a complete line of products to treat specific menopausal symptoms such as hot flashes, memory loss, mood swings, urinary tract infections, and reduced sexual desire. These products effectively treat these symptoms without harmful side effects. Even more importantly, the wisdom of Maharishi Ayurveda offers practical and effective ways to prevent these disorders from happening at all.
What is Soma?
Soma has to do with the finest relative or celestial value that exists in all of nature including the human physiology.
Soma has a cooling, nourishing influence on the physiology, and is associated with lunar energy. In fact, soma is another word for "essence of the moon. Soma, or lunar energy, must be balanced with agni, or the solar energy that is associated with the sun in nature and with the digestive fire in the human body.
Here's one example of how these two forces work together in the body. When you eat an apple, the apple gets crushed by agni in the digestive process, and becomes the liquid nutritive fluid (rasa dhatu). As the nutritive fluid is further metabolized by the body, it becomes more and more refined. At some point, in the gaps between the dhatus (tissues), it becomes soma.
Ideal health means maintaining a balance between the cooling, nurturing, lunar energy of soma and the warm, metabolic and cleansing energy of agni. Women naturally have more soma in their physiology than men, and thus it is very important to maintain a good quantity of soma in the female physiology in order to maintain women's health.
Q: In the West menopause is likened to a disease, with women often under a physician's care for treatment. Is the ayurvedic approach similar or does a planned program of self-care help you go through menopause relatively without discomfort?
A: In the ayurvedic tradition, menopause is viewed not as a disease but as a transitional imbalance. Just as imbalances in the body arise due to the change of seasons, changes in weather, and the changing influence of the sun, moon and planets, menopause is a natural transition in a woman's life.
And just as Maharishi Ayurveda explains how to avoid imbalances in other transitional periods of life, it explains how to avoid imbalances during menopause.These transitions from one stage of life to the next are natural, and menopause itself is manageable through Maharishi Ayurveda. To use an analogy, there may be bumps in the road due to changing from one sort of pavement to another, but if you know the bumps are coming, you can take precautions to slow down so you don't blow out your tires.
In the same way, in daily life change is unavoidable. Maharishi Ayurveda offers concrete lifestyle and dietary guidelines to make those transitions smooth. This is the value of the seasonal routine (ritucharya), and this is the value of the special ayurvedic guidelines for the other changes in a woman's life: puberty, pregnancy, postpartum and menopause. They make the transitions happen smoothly, without discomfort or disease.
So the answer to your question is yes, the knowledge of Maharishi Ayurveda offers a complete self-care program for avoiding menopausal discomfort.
Q: Why do so many women in the West experience menopause-related symptoms such as hot flashes, loss of memory, emotional imbalance, and loss of sexual drive?
A: That is a good question. The main thing to understand is that menopause takes place during the transition between the Pitta stage of life and the Vata stage of life. Maharishi Ayurveda outlines three stages of life (called Kala in Sanskrit) for both men and women: Kapha Kala forms the first trimester, when Kapha dosha predominates and the body's structure is developed to maturity. Next is Pitta Kala or the adulthood trimester, when Pitta dosha is predominant and most people achieve their peak in terms of productivity and creativity. Vata Kala, the third trimester, occurs at the end of life, and is predominated by Vata dosha.
Because menopause occurs towards the end of Pitta Kala and the beginning of Vata Kala (the exact age a woman experiences these transitions varies), it is common for a menopausal woman to experience both Vata and Pitta related imbalances. For instance, menopausal complaints such as insomnia, memory lapses, anxiety, vaginal dryness, and aging skin are all related to an imbalance in Vata dosha. Pitta-related imbalances are experienced in menopause as hot flashes, urinary tract infections, anger, irritability, hyperacidity, and skin breakouts and rashes.
If a woman already has a significant Pitta or Vata imbalance in the years before menopause, her symptoms are likely to be much, much worse.
Another factor leading to menopausal imbalances is the accumulation of the digestive impurities called ama in the physiology, often caused by eating a diet of fast foods, foods with chemicals and preservatives, and packaged, canned, frozen or left-over foods. Ama blocks the channels that transport nutrition to the cells and remove waste from the body, and thus ama contributes to disease and aging, including menopausal problems.
Basically if a woman has had problems in the years before menopause with accumulation of ama then the symptoms of menopause are likely to be worse. A third factor is the misuse and overuse of the mind, body, emotions, or senses. Basically, this happens when a woman strains her mind too much, is under too much ongoing stress or pressure, or is doing work that is too "heavy" for her body, or is under tremendous emotional stress.
So if a woman enters menopause with a Vata or Pitta imbalance, or with the accumulation of ama, or having strained her emotions, mental faculties, physical body or senses through misuse or excessive use--then these pre-existing imbalances will combine with the natural fluctuations in hormones that take place during menopause. The result will be the symptoms that we recognize as hot flashes, loss of memory, emotional imbalance, weight gain, urinary infections, vaginal dryness, loss of sexual desire, and sleep problems.
Unfortunately, these causal factors are found more often in the West, or in women who are living a fast-paced lifestyle as in the West. When I was practicing in India, the women in the villages did not have the same problems of menopause that I am seeing in my practice in the West. There is an interesting story that illustrates this difference. In the village where I lived in India, there were two identical twin sisters.
One stayed in the village all her life, and the other moved to New Delhi, the Indian capital, with her husband. When these women reached menopausal age, the sister who stayed in the village had a smooth transition with no symptoms. The sister who had moved to New Delhi eventually consulted my father because she was suffering many complications of menopause, due mainly to her faster-paced, more stressful lifestyle and lesser attention to a proper diet and daily routine.
Q: This is fascinating, that menopausal symptoms are a symptom of the imbalances of our culture as well as the time of life itself. What's the best way to prepare for menopause and prevent these imbalances from happening?
A: The most important thing is to prevent Pitta and Vata imbalances and to keep the body free of ama before menopause begins. First of all, it's important to understand that not all women will get the same symptoms. Some will have more hot flashes, some more mood swings, others a memory problem, and others a loss of libido. Very few will have all the symptoms. And some women will have no symptoms at all.
The reason for this variation, even though all women experience the same reduction in estrogen at the time of menopause, is that there are other factors in play, as we have already mentioned. If someone is of Pitta constitution, or if they are eating foods that cause a Pitta imbalance or living a lifestyle that creates those imbalances, they are going to experience more Pitta-related symptoms such as hot flashes and mood swings. On the other hand, if the person has a Vata imbalance due to having more Vata in their constitution or eating more Vata foods and living a Vata-aggravating lifestyle, then they will experience more Vata-related symptoms, such as memory loss and vaginal dryness.
So it's important to identify the etiological (causal) factors behind the symptoms. You could say that the main cause is the drop in hormones due to menopause, and certainly this is a major transition in a woman's life. But if the cause is only a drop in hormones, why isn't every woman getting the same symptoms? An intelligent woman can see that there also has to be some imbalance there in order for specific symptoms to manifest. And that is what you need to identify, whether it's a Vata or Pitta imbalance, and you need to stop doing those things that are causing the imbalance.So if you start to have any of the Pitta-based problems of menopause, be sure to follow a Pitta-pacifying diet. Avoid foods that are spicy, such as chilies, cayenne and black mustard seed. Salty foods and foods that are sour, such as yogurt (unless it is diluted and sweetened in a drink called lassi) and sour fruits such as ketchup, mustard, and other salad dressings and condiments made with vinegar should also be avoided.
Favor foods that are bitter, astringent and sweet, as these are cooling to Pitta dosha. Bitter and astringent foods include most vegetables. Sweet foods include rice, milk and cream, sweet lassi, wheat products, pasta. Sweet, juicy fruits such as pears and plums also pacify Pitta dosha. Cook with Pitta-reducing spices, such as cinnamon, coriander, cardamom, fennel and small amounts of cumin seed.
If you start to have some Vata-related symptoms of menopause such as memory loss or vaginal dryness, you'll want to work at bringing Vata dosha back into balance. For this, you'll want to eat foods that are cooked, warm, and unctuous (meaning that they have a small amount of good fats such as ghee and olive oil). Eat foods that are sweet, sour and salty, as this balances Vata dosha.
Apana Vata, which governs the genito-urinary tract, elimination, and menstruation, is a key area to attend to when preparing for menopause. Drink plenty of warm water throughout the day. Eat plenty of cooked, leafy greens, as this helps elimination and is also a good source of calcium. For both Pitta and Vata imbalances, a breakfast of cooked apples and prunes and figs is a good way to start the day, as it balances the doshas and cleanses the digestion.
In addition to balancing Pitta and Vata dosha, it's important to keep your digestion strong and free of ama. All of the above suggestions will help with this, In addition, avoid eating foods that are packaged, processed, frozen, canned or left over. Eat organic foods that are cooked fresh each day. The bulk of your diet should consist of whole grains, fresh fruits and vegetables, and legumes and light dairy products such as milk, lassi or panir for protein. This type of light but nourishing diet will aid your digestion and avoid the build-up of ama. Avoid heavy foods such as meat, cheese, yogurt and frozen desserts like ice cream, especially at night.
Q: And are there any lifestyle tips for preparing for menopause?
A: Yes. Sleep is an important area of concern for the woman entering menopause, because both Vata and Pitta imbalances can cause sleep problems that will only make menopausal imbalances worse. To keep both doshas in balance and to sleep more deeply at night, be sure you're in bed before 10:00 p.m. and that you arise before 6:00 a.m. This is the time of night when sleep comes easier and is more restful. If you stay awake past 10:00, it will be harder to fall asleep, and you'll also increase any Pitta imbalance, because 10:00 p.m. to 2:00 a.m. is the Pitta time of night, when the body needs to be at rest in order to cleanse and purify itself.
The morning abhyanga or ayurvedic oil massage is extremely important for preventing menopausal problems. Use the Youthful Skin Oil for Women. This oil is designed to increase circulation, calm Vata dosha, and prov ide needed moisture to the skin. For both Pitta and Vata dosha, it's important not to skip meals, and to eat your main meal at noon, when digestion is the strongest. Try to eat at the same time every day, and go to bed and wake up at the same time. And be sure to get lots of rest during your menstrual cycle as you approach menopause, because this will keep Apana Vata in balance and avoid more serious complications of menopause. Daily exercise (gentle for Vata and not too overheating for Pitta) is also important for keeping all doshas in balance. F inally, practice of the Transcendental Meditation® program is an effective way to keep the doshas in balance, to keep the mind clear and focused, and to calm the emotions and dissolve stress.
Q: You've given us a clear picture of what to do to prevent menopausal problems. What should a woman do during menopause?
A: All of these dietary and lifestyle suggestions that I just described to help prevent menopausal problems will also help keep Pitta and Vata dosha in balance once menopause begins.
Q: I understand that you have developed a completely new line of products for menopause called the Graceful Transition line of nutritional supplements. Can you tell us about this targeted line of products for menopause?
A: The Graceful Transition line as a whole is designed to prevent and address the imbalances related to menopause. It provides both general support and targets specific imbalances that women experience before, during and after menopause. The Graceful Transition line includes these products: Hot Flash Relief, Midlife for Women 1, and Midlife for Women2. In addition, the program includes dietary and lifestyle recommendations to correct specific imbalances during menopause.
The entire program is targeted especially for women of the West: who have the Western physiology, live in that environment, or work in that culture. It addresses the dietary needs, lifestyle and stress levels of women who live a fast-paced life. This program is designed to promote the overall emotional, physical and mental health of women. It helps keep the body free of ama and maintains the balance between soma (lunar energy) and agni (solar energy).
Q: That sounds like an amazingly comprehensive program. Can you tell us first of all what causes each type of imbalance and how each formula from the Graceful Transition line can help?
A: Certainly. Let's start with hot flashes. Hot flashes are caused when too much Pitta dosha accumulates in the body and at the same time ama blocks the channels (srotas). This causes the circulation of heat to become uneven, which women experience as hot flashes. Hot flashes, you could say, are the body's attempt to release heat that has accumulated due to blocked channels.
There is another factor that is highly important here, and that is the influence of soma on a woman's physiology. Soma is the cooling, nourishing substance related to lunar energy that is more predominant in a woman's physiology (see box for more detailed explanation). When, due to Vata and Pitta imbalances, the cooling soma decreases, this contributes to chronic hot flashes. Hot Pitta burns soma and high Vata dries it. When the channels are clogged and the release of heat in the body gets obstructed, then heat builds up and eventually gets released through uncomfortable hot flashes or night sweats.
Once there is this level of Pitta imbalance, and the damage has been done, so to speak, then what is needed is an herbal product to reduce Pitta in the deeper tissues of the body, such as the muscle and fat tissues. In addition, the microcirculatory channels of all the tissues (dhatus) and the waste products (malas) need to be cleansed. It's necessary to regulate the heat throughout the body and the brain as well. Most importantly, the connection between the the mind and body and the mind and the heart need to be re-established. In ayurvedic terms, this relationship between mind and heart is governed by Sadhaka Pitta, the subdosha that regulates the emotions and their effect on the heart, and Prana Vata, the subdosha that regulates the mind and senses. Finally, in chronic situations, soma must be increased, because the burning effect of hot flashes has reduced it to critical lows.
Hot Flash Relief is designed to repair all of these imbalances in order to cool the body and reduce hot flashes during menopause.
Q: That's remarkable, that Hot Flash Relief has been designed to take into account all these different causes of hot flashes. Can you tell us something about the herbs in the formula and how they achieve these effects?
A: Let's look at the first benefit this formula imparts: to reduce Pitta in the deeper tissues of the body. To reduce Pitta imbalance in the deeper tissues, the fat (medha) and muscle (mamsa) tissues, we added the ayurvedic herbs Shatavari, Indian Asparagus, Indian Sarsaparilla, Khus Khus Grass, Water Lily, Sandalwood, Indian Tinospora, Cabbage Rose, and Mica Bhasma. These herbs, when combined, perform an important task. They go deep into the fat and muscle tissues and remove the heat that has been stored there.
There's a very interesting story related to one of these ingredients, Water Lily, which to me illustrates how this wisdom of Maharishi Ayurveda is so profound. In ancient times, the great seers were aware that there were many herbs to increase soma and reduce heat in the deep tissues of the body. But they also knew that there was only one herb that is ideal to increase soma production in women, and that herb is the Water Lily.
Now, every herb has its own intelligence, its own purpose. Some plants are receptors for solar energy (agni), and thus have a heating effect on the human physiology. Other plants are receptors for lunar energy (soma), and thus have a cooling, nourishing effect. To understand how this works, think of a chili pepper. Nature has given it a receptor, you could say, that allows it to store solar energy. If you allow a green chili to mature until it is red in color, it will store more solar energy and we experience this as a hotter taste.
I learned a valuable lesson about the intelligence of herbs when I was interning with my father. We lived near a pond in which the Water Lily and the Red Lotus grew. The Red Lotus is large and red, and its petals are open during the day and closed at night. The Water Lily, on the other hand, opens its petals at night and closes them during the day.
My father pointed out that both lilies are cool by nature because they live in the water and derive their nourishment from the water. So both are good for pacifying Pitta on the deeper tissues, as is needed in the Hot Flash Relief formula. But if you also need an herb that increases soma, then the best choice is the Water Lily, because its petals are open during the night and closed during the day. The fact that it is open to the moon and closed to the sun makes it a receptor of lunar energy, and the best herb to increase soma in the feminine physiology.
You can see from this illustration that if you follow the traditional, proven guidelines of Maharishi Ayurveda, the formulation ends up being unique and highly effective.
Q: That's a fascinating story. What other herbs are used in this formula?
A: Other herbs such as Long Pepper, Indian Sarsaparilla, Turbinella rapa Bhasma and Cumin seed cleanse ama from the microchannels. Indian Tinospora, Shatavari, Coral (Corallium Rubrum) and Licorice nourish the connection between mind and body and mind and heart. Khus Khus Grass (Vetiver), Sandalwood and Mica Bhasma maintain proper heat regulation.
As far as dietary tips for reducing hot flashes, follow a Pitta pacifying diet. Don't eat anything that aggravates Pitta. Favor more sweet, juicy fruits, Rose Petal Preserve, and start the day with a stewed apple.
Keep your home environment cool, pleasant and loving. Fill your garden and home with roses. For daily abhyanga (ayurvedic oil massage), use 50% Youthful Skin Oil and 50% Cool Sensation Oil. This will calm and balance the emotions and support coordination of body, mind and heart.
Q: Can you tell us what causes other Pitta-related imbalances, such as mood swings?
A: Changing hormones can contribute to emotional ups and downs during menopause, and this physiological change can be magnified by special problems such as work pressures, children leaving the home, the burden of caring for ailing parents, and financial and marital problems. When emotional stress becomes chronic, even the brain chemicals can be affected, leading to feelings of depression.
Sadhaka Pitta, which governs the emotions and their effect on the heart, is often thrown out of balance when Pitta dosha becomes aggravated, creating sudden mood swings and a critical attitude towards loved ones.
To counteract mood swings, I'd recommend taking Stress Free Emotions along with a Pitta pacifying diet. If you feel critical or upset, try eating a sweet, juicy pear or take a teaspoon of Rose Petal Preserve. It's very important to take care of emotional imbalances when they first appear, because if left untreated they can cause major problems and even lead to early menopause. So it's very important to keep Sadhaka Pitta in balance at all times.
The various herbs in Stress Free Emotions combine to do three things: enhance coordination between mind and emotions, cleanse the channels between heart and mind, and nourish the heart and mind.
Q: What is the best way to approach multiple symptoms? Can a woman take all of these formulas at one time?
A: If a woman has multiple symptoms, she should try to find out which symptom occurred first. Then she should try to address that problem first, and make the recommended lifestyle and dietary changes along with taking the formulation.
What often happens is that one imbalance creates additional imbalances, with the root imbalance causing other symptoms to manifest. So as a general rule in Maharishi Ayurveda, we address the symptom and underlying imbalance that occurred first, since it is often the cause of later problems. For instance, if someone is hungry and then gets a headache, it would be wise to eat a meal first, instead of just popping a pain-relieving pill. The secondary symptom is often related to the first symptom, in the same way that the headache is related to hunger.
In general, take only two of the Graceful Transition formulas at one time, and in special cases up to three. But if you feel you have three or more symptoms, it's best to consult a physician trained in Maharishi Ayurveda, who can determine the primary cause through nadi vigyan (pulse diagnosis). This is also a good idea if you are taking other herbal formulas or medications.
An important part of this program is knowledge, and I'd highly recommend the newly released book, A Woman's Best Medicine for Menopause: Your Personal Guide to Radiant Good Health Using Maharishi Ayurveda, by Nancy Lonsdorf, M.D. This book gives a deep understanding of menopause, its imbalances, and the causes of specific symptoms. It also outlines a complete self-care program for taking care of those symptoms and removing the imbalances at their source.
Q: How do Midlife for Women I and II fit in with these Graceful Transition targeted menopause formulas? And what about taking Maharishi Amrit Kalash with these products?
A: I'm glad you asked because this is important to clarify. Midlife for Women I and II should be taken along with the new targeted formulas from the Graceful Transition lines. Midlife for Women I (for preparing for menopause) and Midlife for Women II (for during menopause) provide overall support. A woman needs both types of nourishment and support--general and specific.
Many women won't have any symptoms, and will be able to stay in balance by just taking Midlife for Women I or II. For women who have specific imbalances, such as hot flashes, mood swings, urinary tract disorders, vaginal dryness or memory loss, they should take both the Midlife for Women I or II plus up to two of the specific formulas.
Maharishi Amrit Kalash is the supreme rasayana, or herbal compound, for overall balance and youthfulness, so it can be taken in addition to two other herbal formulas.
Q: Osteoporosis is, of course, another problem often associated with menopause. Can you tell us something about the Calcium Support formula?
A: The Calcium Support formula is a vegetarian source of calcium that is easily absorbable and safe. Since one of the problems with calcium supplements is that they are often not absorbed by the body, this formula focuses on absorption, and contains herbs that enhance absorption of calcium. It also enhances the metabolic mechanisms between fat and bone tissue, so the bone tissue can actually utilize the calcium and other nutrients supportive to the bone. This high absorbability makes Calcium Support a unique product on the market today. Many commercial varieties are digested but not absorbed by the body, which creates a strain on the kidneys to remove the excess calcium through the urinary tract.
Another important feature of Calcium Support is that it is lead-free. Many commercial calcium supplements today contain lead, which is harmful to the body. Calcium Support contains Pearl Bhasma, which is one of the richest sources of calcium mentioned in the traditional ayurvedic texts. It and the other natural sources of calcium are easily absorbable and natural.
Q: Should you take the Calcium Support along with the Graceful Transition supplements?
A: Women of any age can take Calcium Support on an ongoing basis as you would a food, one tablet twice a day, without counting it as one of the Graceful Transition formulas that you take.
Because Herbal Calcium Absorb contains herbs to enhance utilization, and because the herbs also increase the absorption of calcium from the food you eat, it is much more effective in supplying needed calcium to menopausal women than the large quantities normally recommended for other types of calcium supplements.
Q: Menopausal women sometimes complain about skin and hair problems such as acne. What are the reasons for these symptoms?
A: One reason is that the decrease in estrogen and the onset of Vata time of life associated with menopause causes the glands to produce less oil and the deeper fat layers to become thinner.
This drying effect of Vata dosha causes the skin to wrinkle and lose its softness.
The surface layer of the skin also thins, and thus many women find that their skin is more sensitive to sunburn, windy and dry conditions, and allergens. That's why women in their fifties are sometimes dismayed to find that they have a case of acne, something they haven't faced since adolescence.
Aging also causes a decrease in circulation and blood flow, so the skin is no longer nourished on deeper levels. This, along with the drying of natural emollients, can cause the skin to look pale and pasty. Fluctuations in hormones also cause collagen to decrease, making the skin less firm and youthful looking.
Q: Do women just have to accept these changes, or is there something that they can do to increase the natural vitality and beauty of their skin?
A: Maharishi Ayurveda offers a wide range of remedies to keep a woman's skin healthy and youthful as she ages. The most important thing is to identify your skin type. Vata skin is delicate, thin, fine-pored and cool when you touch it. When out of balance, it is more prone to dryness, roughness, a gray or wan color, wrinkles and early aging. Pitta skin is usually fair and sensitive, with a tendency to freckles, moles, pinkish or reddish color. When out of balance it can develop sunspots, rashes, and breakouts. Kapha skin is usually soft, oily, thick, and darker in color. When out of balance, it can develop enlarged pores, blackheads and pimples, moist types of eczema and water retention.
For Vata skin, you'll want to moisturize your skin from the inside and out. Drink several glasses of pure water a day. Eat plenty of sweet, juicy fruits. Follow a Vata pacifying diet. Because Vata skin is delicate, you'll want to avoid harsh cleansers or products with chemical ingredients. The Youthful Skin Massage Oil is especially soothing to Vata, and helps nourish and soothe the skin.
For Pitta skin, which tends to be extremely sensitive, you'll also want to avoid harsh chemical ingredients. Cooling foods and tastes are best for your diet. Include Ghee and Rose Petal Preserve in your diet.
The Youthful Skin products are ideal for rejuvenating dry and aging skin and making it youthful again, and are completely free of harmful additives and preservatives. In fact, the Youthful Skin Cream is comprised of 9.5% herbal extract, which is truly an unheard of percentage. Most skin creams that are labeled "herbal" or "natural" contain only .025-1% herbal extracts.
Youthful Skin Cream has been tested in an independent laboratory with impressive results.
After two months, skin thickness increased by an average of 14.59%, which is a remarkable result from an all-natural cream. Wrinkles were reduced an average of 33% in the first month, and by 40% in just three months. Firmness, clarity and radiance, and moisturizing of the skin all were also substantially improved.
One reason that Youthful Skin Cream is so effective in moisturizing the skin is that the herbs open the channels and allow moisture to be conveyed to the deepest layers of the skin. Youthful Skin Cream, even though applied from the outside, actually improves the metabolism of the skin and opens the channels so it can show the results of being moisturized from the inside (by drinking water) and from the outside with the application of the cream.
The Youthful Skin Herbal Tablets are also a big help for menopause-related skin problems, because they promote contentment and serenity even in the face of stressful challenges. This formula also nourishes the deepest layer of the skin, the rohini layer, which means that it helps replenish and rebuild the tissues and fluids necessary for healthy skin.
Maharishi Ayurveda Products International, Inc.
Friday, July 28, 2006
HRT Raises Risk for Specific Breast Cancers
THURSDAY, Feb. 16 (HealthDay News) -- When taken for more than five years, estrogen-progestin hormone replacement therapy (HRT) is associated with a more than two-fold higher risk of lobular breast cancer or tubular breast cancer, compared with the more common ductal breast cancer, Swedish researchers report.
According to the American Cancer Society, about two-thirds of breast cancers are ductal malignancies, arising in the breast ducts. A smaller percentage of breast cancers are categorized as either lobular -- arising in milk-producing glands called lobules -- or tubular, meaning the cancer itself produces small glands and tubules resembling mammary ductules. Lobular and tubular breast cancers usually have a somewhat better prognosis than ductal cancers.
Reporting Thursday in the journal Breast Cancer Research, researchers at the Karolinska Institut in Stockholm found that HRT, typically given to help reduce menopausal symptoms, is associated with a greater risk of developing tubular rather than ductal cancer. The study also confirms previous findings that the therapy is associated with a greater risk of lobular cancer vs. ductal cancer.
The study included 1,888 women with ductal cancer, 308 women with lobular cancer, and 93 women with tubular cancer. They were matched with a control group of more than 3,000 women without breast cancer.
Both the breast-cancer patients and the women in the control group provided information on their medical history, health status and use of menopausal therapies.
Women who used medium potency estrogen-progestin combination therapy had a higher risk of either lobular or tubular breast cancer than of ductal cancer, compared with women who did not use hormone therapy. Women who used the therapy for more than five years had a higher risk, the study authors found.
They also found that other factors, such as body mass index, number of births, and age at menopause, were associated with a similar risk of developing these three forms of breast cancer.
More information
The U.S. National Heart, Lung, and Blood Institute has more about estrogen-progestin therapy.
Last reviewed: 02/16/2006 Last updated: 02/16/2006
According to the American Cancer Society, about two-thirds of breast cancers are ductal malignancies, arising in the breast ducts. A smaller percentage of breast cancers are categorized as either lobular -- arising in milk-producing glands called lobules -- or tubular, meaning the cancer itself produces small glands and tubules resembling mammary ductules. Lobular and tubular breast cancers usually have a somewhat better prognosis than ductal cancers.
Reporting Thursday in the journal Breast Cancer Research, researchers at the Karolinska Institut in Stockholm found that HRT, typically given to help reduce menopausal symptoms, is associated with a greater risk of developing tubular rather than ductal cancer. The study also confirms previous findings that the therapy is associated with a greater risk of lobular cancer vs. ductal cancer.
The study included 1,888 women with ductal cancer, 308 women with lobular cancer, and 93 women with tubular cancer. They were matched with a control group of more than 3,000 women without breast cancer.
Both the breast-cancer patients and the women in the control group provided information on their medical history, health status and use of menopausal therapies.
Women who used medium potency estrogen-progestin combination therapy had a higher risk of either lobular or tubular breast cancer than of ductal cancer, compared with women who did not use hormone therapy. Women who used the therapy for more than five years had a higher risk, the study authors found.
They also found that other factors, such as body mass index, number of births, and age at menopause, were associated with a similar risk of developing these three forms of breast cancer.
More information
The U.S. National Heart, Lung, and Blood Institute has more about estrogen-progestin therapy.
Last reviewed: 02/16/2006 Last updated: 02/16/2006
Study That Discredited HRT Was Flawed, Experts Say
(HealthDay News) -- The Women's Health Initiative was a landmark study involving 27,000 participants that caused many women to discontinue their use of hormone replacement therapy (HRT).
Researchers halted the study in 2002 after they found the regimen entailed more health risks -- most notably an increased risk for breast cancer and stroke -- than benefits.
But an expert who has conducted a new critique of the study contends it had major methodological flaws.
"I looked at the way they designed the study, and they did make some major mistakes," said Dr. Edward L. Klaiber, a consultant endocrinologist at the University of Massachusetts Medical Center. He is the lead author of the article, published in the December issue of Fertility and Sterility.
The estrogen/progestin arm of the Women's Health Initiative (WHI) was halted when researchers found the regimen increased the risk of invasive breast cancer and blood clots in the legs and lungs, in addition to not protecting women from heart disease and strokes.
Then, in 2004, the estrogen-only phase of the study was stopped because it was linked to an increased risk of stroke, with no reduction in women's risk for heart disease.
In the wake of the WHI study, the American Heart Association recommended that long-term hormone therapy not be used for cardiovascular disease prevention and that its use for other reasons "should be cautiously considered with the advice of a physician."
According to Klaiber, in the estrogen/progestin arm, 73 percent of the women -- who averaged 63 years of age -- had never taken HRT before. In the estrogen-only group, 52 percent of those women (also averaging 63 years of age) had not taken hormone therapy before.
Klaiber's major criticism of the WHI: "They were putting women in their 60s and 70s who hadn't been on hormones on hormones for the first time," he said. Because these women were older, they were already at greater risk of cardiovascular problems, he reasoned.
Another flaw? One of the two regimens in the study "used daily progesterone," said Klaiber, who prefers non-continuous administration of progesterone.
"That hormone pattern had never been tested at that time for its effect on breast cancer and heart disease," Klaiber said. The other regimen, administered to women who had had a hysterectomy, used only estrogen.
Klaiber argues that hormone replacement therapy in other doses or delivery forms is not only safe, but still has a positive health effect. He pointed to previous findings from the large-scale Nurses' Health Study, in which women were placed on hormone therapy earlier -- in their 40s and 50s -- and did not take the combination continuously. That study found a heart-protective effect, he said.
"The women in the Nurses' Study were not taking progestin daily," Klaiber said. "They took it cyclically, usually 10 to 12 days a month instead of daily."
The new review is basically a rehash of previous criticisms, said Dr. Nieca Goldberg, chief of women's cardiac care at Lenox Hill Hospital in New York City.
"It's a critique," she said. "It has no new information."
"Many of these issues were brought up a couple years ago," she added. "In order for them to prove any of these other things -- such as other forms [of HRT] would be better -- they need to do a study." Goldberg said Klaiber's article won't change the way she practices.
Klaiber agreed that more study is needed. He said one study, currently underway, is evaluating the worth of earlier intervention with hormones as a way to protect the heart.
The Massachusetts expert said he's convinced that transdermal estrogen, given in patch form, is superior to oral estrogen. "Oral estrogen passes through the liver and stimulates the blood-clotting factors too much, leading to heart attacks," he said. Not every woman who uses oral hormones will get a heart attack, he emphasized, but women who already have cardiovascular problems might be at raised risk.
Until more studies are done on other forms of therapy, Klaiber said, "the best evidence we have comes from the earlier studies." And those include regimens of estrogen and non-continuous progestin, he said.
More information
To learn more about hormone therapy, visit the Mayo Clinic.
Researchers halted the study in 2002 after they found the regimen entailed more health risks -- most notably an increased risk for breast cancer and stroke -- than benefits.
But an expert who has conducted a new critique of the study contends it had major methodological flaws.
"I looked at the way they designed the study, and they did make some major mistakes," said Dr. Edward L. Klaiber, a consultant endocrinologist at the University of Massachusetts Medical Center. He is the lead author of the article, published in the December issue of Fertility and Sterility.
The estrogen/progestin arm of the Women's Health Initiative (WHI) was halted when researchers found the regimen increased the risk of invasive breast cancer and blood clots in the legs and lungs, in addition to not protecting women from heart disease and strokes.
Then, in 2004, the estrogen-only phase of the study was stopped because it was linked to an increased risk of stroke, with no reduction in women's risk for heart disease.
In the wake of the WHI study, the American Heart Association recommended that long-term hormone therapy not be used for cardiovascular disease prevention and that its use for other reasons "should be cautiously considered with the advice of a physician."
According to Klaiber, in the estrogen/progestin arm, 73 percent of the women -- who averaged 63 years of age -- had never taken HRT before. In the estrogen-only group, 52 percent of those women (also averaging 63 years of age) had not taken hormone therapy before.
Klaiber's major criticism of the WHI: "They were putting women in their 60s and 70s who hadn't been on hormones on hormones for the first time," he said. Because these women were older, they were already at greater risk of cardiovascular problems, he reasoned.
Another flaw? One of the two regimens in the study "used daily progesterone," said Klaiber, who prefers non-continuous administration of progesterone.
"That hormone pattern had never been tested at that time for its effect on breast cancer and heart disease," Klaiber said. The other regimen, administered to women who had had a hysterectomy, used only estrogen.
Klaiber argues that hormone replacement therapy in other doses or delivery forms is not only safe, but still has a positive health effect. He pointed to previous findings from the large-scale Nurses' Health Study, in which women were placed on hormone therapy earlier -- in their 40s and 50s -- and did not take the combination continuously. That study found a heart-protective effect, he said.
"The women in the Nurses' Study were not taking progestin daily," Klaiber said. "They took it cyclically, usually 10 to 12 days a month instead of daily."
The new review is basically a rehash of previous criticisms, said Dr. Nieca Goldberg, chief of women's cardiac care at Lenox Hill Hospital in New York City.
"It's a critique," she said. "It has no new information."
"Many of these issues were brought up a couple years ago," she added. "In order for them to prove any of these other things -- such as other forms [of HRT] would be better -- they need to do a study." Goldberg said Klaiber's article won't change the way she practices.
Klaiber agreed that more study is needed. He said one study, currently underway, is evaluating the worth of earlier intervention with hormones as a way to protect the heart.
The Massachusetts expert said he's convinced that transdermal estrogen, given in patch form, is superior to oral estrogen. "Oral estrogen passes through the liver and stimulates the blood-clotting factors too much, leading to heart attacks," he said. Not every woman who uses oral hormones will get a heart attack, he emphasized, but women who already have cardiovascular problems might be at raised risk.
Until more studies are done on other forms of therapy, Klaiber said, "the best evidence we have comes from the earlier studies." And those include regimens of estrogen and non-continuous progestin, he said.
More information
To learn more about hormone therapy, visit the Mayo Clinic.
Beyond HRT is a product designed to promote healthy hormones in both men and women.
FRIDAY, Sept. 16 (HealthDay News) -- The increased risk of breast cancer known to be associated with the use of hormone replacement therapy (HRT) applies to all ethnicities, a new study finds.
Ever since the Women's Health Initiative (WHI) study was halted in 2002, after investigators found that the women taking HRT had a higher incidence of heart attacks, strokes, blood clots and breast cancer, experts have known about the increased health risks.
But one of the unresolved issues has been whether women of all races were equally affected, since the majority of the WHI participants were white, explained study co-author Malcolm Pike, a professor of preventive medicine at the University of Southern California's Keck School of Medicine. His report appears in the Sept. 16 online issue of the International Journal of Cancer.
However, based on the new study, Pike said, the firm conclusion is that "every one of these ethnic groups has the same risk of breast cancer from HRT."
Pike's study evaluated more than 55,000 menopausal American women taking part in the Multiethnic Cohort Study. That study included more than 215,000 men and women, aged 45 to 75 at the start of the study who were living in Hawaii or California in 1993. The women included whites, blacks, Hawaiians, Japanese-Americans and Latin Americans. "The women told us their contraceptive history, their pregnancy history, what hormones they took post-menopause," Pike said.
Current use of the estrogen-progestin therapy was associated with a 29 percent higher risk of breast cancer after five years of use, he found. The association held for women in all ethnic groups. Current use of estrogen-only therapy was associated with a 10 percent higher risk of breast cancer after five years of use, and this was found in all ethnic groups except for blacks.
The researchers also found that leaner women -- those with a body mass index (BMI) below 25, had a slightly higher relative risk of getting breast cancer than the heavier women, although the heavier women were also at increased risk. Although the researchers couldn't pinpoint the reason for the finding, Pike did have a theory.
"The bigger you are postmenopausally, the more estrogen you [continue] to make," he said. That's because the more fat cells a woman has, the more estrogen she produces.
A woman who weighs 180 pounds, for example, is probably making as much estrogen herself as the breast positively reacts to, Pike said. "These women are at a saturation point."
But the woman who weighs, say, 130 pounds or less gets more of an effect from supplementary estrogen, he said, perhaps accounting for their increased risk.
Studies following the halting of the WHI have been plentiful, all evaluating different aspects of risk. A study published last month in the British Medical Journal found that the risk of breast cancer declines with age if a woman is not taking HRT. But if she does take HRT, that risk starts to climb. If therapy is stopped, however, the risk returns to that of a woman of the same age who has never used HRT, the researchers found.
Another expert, Roshan Bastani, associate dean for research at the University of California Los Angeles School of Public Health and Jonsson Comprehensive Cancer Center, praised the new research.
"I think it's a well-done study," she said. "And it is important, particularly because they were able to include data from large numbers of people from many ethnic groups."
For women, the study provides more valuable information, but each woman must still take into account her own symptoms, medical history and family background when deciding whether to take hormones after menopause, Pike and Bastani agreed.
"What they need to do," Bastani said, "it to understand the risks and then assess whether they are willing to take the risk."
For instance, she said, if a particular woman is told taking hormones increases her risk of breast cancer or other disease by, say, 10 percent, she should ask what her "baseline" risk is, which depends on factors such as family background and medical history. If the baseline risk is just 1 percent or 2 percent, an increased risk is not a lot compared to a baseline risk of 50 percent or 80 percent.
"If you want to take HRT to deal with problems at menopause, it's perfectly reasonable," Pike said, as long as the treatment is limited. It's difficult, he said, to put an absolute number of years on that advice.
The best course, said Pike, is to keep the amount of progestin "to an absolute minimum."
"What a woman wants to do is discuss with her physician -- can she use the minimum amount of estrogen to control her hot flashes, and how frequently does she need to take progestin?" he said.
More information
To learn more about breast cancer, visit the American Cancer Society.
Last reviewed: 09/16/2005 Last updated: 09/16/2005
Ever since the Women's Health Initiative (WHI) study was halted in 2002, after investigators found that the women taking HRT had a higher incidence of heart attacks, strokes, blood clots and breast cancer, experts have known about the increased health risks.
But one of the unresolved issues has been whether women of all races were equally affected, since the majority of the WHI participants were white, explained study co-author Malcolm Pike, a professor of preventive medicine at the University of Southern California's Keck School of Medicine. His report appears in the Sept. 16 online issue of the International Journal of Cancer.
However, based on the new study, Pike said, the firm conclusion is that "every one of these ethnic groups has the same risk of breast cancer from HRT."
Pike's study evaluated more than 55,000 menopausal American women taking part in the Multiethnic Cohort Study. That study included more than 215,000 men and women, aged 45 to 75 at the start of the study who were living in Hawaii or California in 1993. The women included whites, blacks, Hawaiians, Japanese-Americans and Latin Americans. "The women told us their contraceptive history, their pregnancy history, what hormones they took post-menopause," Pike said.
Current use of the estrogen-progestin therapy was associated with a 29 percent higher risk of breast cancer after five years of use, he found. The association held for women in all ethnic groups. Current use of estrogen-only therapy was associated with a 10 percent higher risk of breast cancer after five years of use, and this was found in all ethnic groups except for blacks.
The researchers also found that leaner women -- those with a body mass index (BMI) below 25, had a slightly higher relative risk of getting breast cancer than the heavier women, although the heavier women were also at increased risk. Although the researchers couldn't pinpoint the reason for the finding, Pike did have a theory.
"The bigger you are postmenopausally, the more estrogen you [continue] to make," he said. That's because the more fat cells a woman has, the more estrogen she produces.
A woman who weighs 180 pounds, for example, is probably making as much estrogen herself as the breast positively reacts to, Pike said. "These women are at a saturation point."
But the woman who weighs, say, 130 pounds or less gets more of an effect from supplementary estrogen, he said, perhaps accounting for their increased risk.
Studies following the halting of the WHI have been plentiful, all evaluating different aspects of risk. A study published last month in the British Medical Journal found that the risk of breast cancer declines with age if a woman is not taking HRT. But if she does take HRT, that risk starts to climb. If therapy is stopped, however, the risk returns to that of a woman of the same age who has never used HRT, the researchers found.
Another expert, Roshan Bastani, associate dean for research at the University of California Los Angeles School of Public Health and Jonsson Comprehensive Cancer Center, praised the new research.
"I think it's a well-done study," she said. "And it is important, particularly because they were able to include data from large numbers of people from many ethnic groups."
For women, the study provides more valuable information, but each woman must still take into account her own symptoms, medical history and family background when deciding whether to take hormones after menopause, Pike and Bastani agreed.
"What they need to do," Bastani said, "it to understand the risks and then assess whether they are willing to take the risk."
For instance, she said, if a particular woman is told taking hormones increases her risk of breast cancer or other disease by, say, 10 percent, she should ask what her "baseline" risk is, which depends on factors such as family background and medical history. If the baseline risk is just 1 percent or 2 percent, an increased risk is not a lot compared to a baseline risk of 50 percent or 80 percent.
"If you want to take HRT to deal with problems at menopause, it's perfectly reasonable," Pike said, as long as the treatment is limited. It's difficult, he said, to put an absolute number of years on that advice.
The best course, said Pike, is to keep the amount of progestin "to an absolute minimum."
"What a woman wants to do is discuss with her physician -- can she use the minimum amount of estrogen to control her hot flashes, and how frequently does she need to take progestin?" he said.
More information
To learn more about breast cancer, visit the American Cancer Society.
Last reviewed: 09/16/2005 Last updated: 09/16/2005
Labels:
advice,
breast cancer,
Menopause,
Menopause Symptomes
Beyond HRT is a product designed to promote healthy hormones in both men and women.
Beyond HRT is a product designed to promote healthy hormones in both men and women. It has a natural way of providing the body with a healthy balance which has been shown to promote a natural immunity towards breast cancer.
The Pueraria Mirifica root is found only in Thailand. Dr. Gordon discovered while visiting Thailand, that this region has the lowest rate of breast cancer in the world and remarkable longevity.
The people who eat the Pueraria Mirifica root have been examined and show virtually no signs of breast cancer, or any early signs of cancer development. Furthermore, they never seem to suffer from menopausal symptoms or osteoporosis.
With this information, Dr. Gordon and Longevity Plus have come together once again to bring you Beyond HRT. This new product contains the Pueraria Mirifica root for an all natural product that can be used to help promote healthy hormones and help prevent breast cancer among people of both genders.*
Beyond HRT helps
Serve as an anti-wrinkle agent for aged and wrinkled skin
Darken white hair, and increase hair growth
Help with memory loss
Increase energy and vigor, more reflexive bodily movements
Alleviate sleep disorders
*These statements have not been evaluated by the FDA. This product is not intended to diagnose, cure or prevent disease. For more information on maintaining a long and healthy lifestyle, please visit Gordon Research Institute.
Suggested Use: Adults - 1 capsule daily for every 60-80 pounds of body weight or as directed by your health professional.
Supplement Facts
Serving Size: one capsule
Ingredient
Amount Per Serving
% Daily Value
Pueraria Mirifica, PE (20 mg miroestrol/100g)
80 mg
*
Milk Thistle, PE (80% Silymarin)
60 mg
*
*Daily Value not established.
Store in a cool, dry place away from sunlight.
KEEP OUT OF THE REACH OF CHILDREN.
The Pueraria Mirifica root is found only in Thailand. Dr. Gordon discovered while visiting Thailand, that this region has the lowest rate of breast cancer in the world and remarkable longevity.
The people who eat the Pueraria Mirifica root have been examined and show virtually no signs of breast cancer, or any early signs of cancer development. Furthermore, they never seem to suffer from menopausal symptoms or osteoporosis.
With this information, Dr. Gordon and Longevity Plus have come together once again to bring you Beyond HRT. This new product contains the Pueraria Mirifica root for an all natural product that can be used to help promote healthy hormones and help prevent breast cancer among people of both genders.*
Beyond HRT helps
Serve as an anti-wrinkle agent for aged and wrinkled skin
Darken white hair, and increase hair growth
Help with memory loss
Increase energy and vigor, more reflexive bodily movements
Alleviate sleep disorders
*These statements have not been evaluated by the FDA. This product is not intended to diagnose, cure or prevent disease. For more information on maintaining a long and healthy lifestyle, please visit Gordon Research Institute.
Suggested Use: Adults - 1 capsule daily for every 60-80 pounds of body weight or as directed by your health professional.
Supplement Facts
Serving Size: one capsule
Ingredient
Amount Per Serving
% Daily Value
Pueraria Mirifica, PE (20 mg miroestrol/100g)
80 mg
*
Milk Thistle, PE (80% Silymarin)
60 mg
*
*Daily Value not established.
Store in a cool, dry place away from sunlight.
KEEP OUT OF THE REACH OF CHILDREN.
Saturday, June 24, 2006
Turmeric helps in breast cancer cure
 Adrienne
AdrienneTurmeric, the medicinal properties of which Ayurveda found millennia ago, is now recognized by modern scientific research as a cure for breast cancer. Its anti toxic properties were also widely known, from ancient times in India. Turmeric is an ingredient in many Ayurvedic medicines.
Houston : Oct 15, 2005. : In what may spell good news for people at advanced stages of breast cancer, researchers have discovered that curcumin - the main ingredient in the common Indian spice turmeric - is an `effective preventive`. Researchers at the University of Texas M.D. Anderson Cancer Centre have found that curcumin, which gives Indian curry its yellow colour; inhibits metastasis in the lungs of mice afflicted with breast cancer.`We know that it`s an effective preventive at low doses, the question is whether larger doses can be therapeutic for disease sufferers,` Dr Bharat Aggarwal, of the experimental therapeutics department at the cancer centre, said. Though study results are early, researchers found the non-toxic natural substance not only repelled progression of the disease to the lungs, but also appeared to reverse the effects of paclitaxel taxol, a commonly prescribed chemotherapy for breast cancer that may trigger spread of the disease with use over a long period of time.`We are excited about the results of the study and the possible implications for taking the findings into the clinic in the next several years,` he said.
Advanced breast cancer is currently a difficult foe to fight with few proven treatments available after surgery, chemotherapy and radiation therapy. Because taxol is so toxic, it activates a protein that produces an inflammatory response that induces metastasis.
Curcumin suppresses this response, making it impossible for the cancer to spread. In fact, researchers found that adding curcumin to taxol actually enhances its effect.
Curcumin breaks down the dose, making the therapy less toxic and, just as powerful while delivering the same level of efficacy.Taxol is currently used as chemotherapeutic agent in breast cancers, but because the drug frequently induces resistance after prolonged use, it is not effective in treating metastatic breast cancer, says Aggarwal.
Researchers studied 60 mice with breast cancer, which were randomly assigned to one of four groups - control group, taxol only, curcumin only and the combination of taxol and curcumin. After the tumours grew to 10 mm in size, they were surgically removed, and the mice were fed powdered curcumin.
Source : PTI
Tuesday, March 21, 2006
Studies Short on Soy Formula Risks
Studies Short on Soy Formula Risks: "Studies Short on Soy Formula Risks
Experts See Little Health Danger With Formula By Todd Zwillich
WebMD Medical News Reviewed By Louise Chang, MD
on Friday, March 17, 2006
More From WebMD
Eating for Two? Get the Right Nutrition
Making the Breastfeeding Decision
Metal in Infant Formula Prompts Recall
March 17, 2006 -- There is not enough scientific data to determine whether or not soy formula consumed by millions of infants poses a health risk, a government panel concluded Friday.
Experts say they have little concern that an estrogen-like substance in soy -- known as genistein -- poses a developmental risk to infants who consume it or whose parents consumed it in soy-based foods.
Still, very few studies have looked at the long-term health effects of soy formula, which is used to feed an estimated 25% of all U.S. infants, the panel says.
Soy has raised concerns not only because of its exploding consumption by U.S. infants and adults but also because studies have shown that genistein can interfere with hormonal function in rats and their offspring.
A variety of toxic effects, including stunted growth, sexual organ abnormalities, and decreased fertilization, have all been observed in laboratory animals. All of the effects appear to be caused by genistein's ability to mimic the effects of natural estrogen. Some researchers also suspect soy of playing a role in reduced breast cancer rates in Japan, where soy consumption is very high.
The committee says it had 'negligible' concern that usual intakes of genistein cause adverse health effects in newborns and infants who consume soy formula, though one expert -- Ruth Etze, MD -- dissented from the conclusion. Etzel, a pediatrician at the Alaska Native Medical Center in Anc"
more info at:
www.dreddyclinic.com
Experts See Little Health Danger With Formula By Todd Zwillich
WebMD Medical News Reviewed By Louise Chang, MD
on Friday, March 17, 2006
More From WebMD
Eating for Two? Get the Right Nutrition
Making the Breastfeeding Decision
Metal in Infant Formula Prompts Recall
March 17, 2006 -- There is not enough scientific data to determine whether or not soy formula consumed by millions of infants poses a health risk, a government panel concluded Friday.
Experts say they have little concern that an estrogen-like substance in soy -- known as genistein -- poses a developmental risk to infants who consume it or whose parents consumed it in soy-based foods.
Still, very few studies have looked at the long-term health effects of soy formula, which is used to feed an estimated 25% of all U.S. infants, the panel says.
Soy has raised concerns not only because of its exploding consumption by U.S. infants and adults but also because studies have shown that genistein can interfere with hormonal function in rats and their offspring.
A variety of toxic effects, including stunted growth, sexual organ abnormalities, and decreased fertilization, have all been observed in laboratory animals. All of the effects appear to be caused by genistein's ability to mimic the effects of natural estrogen. Some researchers also suspect soy of playing a role in reduced breast cancer rates in Japan, where soy consumption is very high.
The committee says it had 'negligible' concern that usual intakes of genistein cause adverse health effects in newborns and infants who consume soy formula, though one expert -- Ruth Etze, MD -- dissented from the conclusion. Etzel, a pediatrician at the Alaska Native Medical Center in Anc"
more info at:
www.dreddyclinic.com
Preventive Mastectomy Satisfying
Preventive Mastectomy Satisfying: "Survey Shows Patients Don't Regret Decision to Remove Disease-Free Breast By Salynn Boyles
WebMD Medical News Reviewed By Louise Chang, MD
on Friday, March 17, 2006
More From WebMD
Breakthroughs in Breast Cancer Treatments
Considering Reconstructive Surgery? Consult Our Guide
What Should Do if You Have the Breast Cancer Gene?
March 17, 2006 -- Breast cancer patients who chose to have a healthy breast surgically removed along with the diseased one tend to be satisfied with the decision, a new survey shows.
Preventive mastectomy is an option for women to reduce risk of developing breast cancer in the other breast, particularly in those with high risk for recurrence.
Bianca Kennedy, now 40, chose it five years ago while being treated for cancer in one breast, and she says she has never regretted it.
Kennedy had undergone a lumpectomy and was in her third month of chemotherapy when her sister was diagnosed with breast cancer for the third time.
'That made my decision easy,' she tells WebMD. 'I told my doctors I wanted both breasts removed. They had not tried to push me into doing it but after I said it was what I wanted they told me they thought it was the wisest thing to do.'
Fears Remain for Many
Women who have cancer in one breast have a three- to fivefold higher risk of developing a second cancer in the opposite breast, and the risk is even higher among women with a family history of the disease.
Studies suggest that the removal of one or both breasts can reduce future breast cancer risk by about 90%, according to the National Cancer Institute.
In the newly published study, 519 women who had a disease-free breast removed while being treated for breast cancer were surveyed along with 61 breast cancer surviv"
more info at:
www.dreddyclinic.com
WebMD Medical News Reviewed By Louise Chang, MD
on Friday, March 17, 2006
More From WebMD
Breakthroughs in Breast Cancer Treatments
Considering Reconstructive Surgery? Consult Our Guide
What Should Do if You Have the Breast Cancer Gene?
March 17, 2006 -- Breast cancer patients who chose to have a healthy breast surgically removed along with the diseased one tend to be satisfied with the decision, a new survey shows.
Preventive mastectomy is an option for women to reduce risk of developing breast cancer in the other breast, particularly in those with high risk for recurrence.
Bianca Kennedy, now 40, chose it five years ago while being treated for cancer in one breast, and she says she has never regretted it.
Kennedy had undergone a lumpectomy and was in her third month of chemotherapy when her sister was diagnosed with breast cancer for the third time.
'That made my decision easy,' she tells WebMD. 'I told my doctors I wanted both breasts removed. They had not tried to push me into doing it but after I said it was what I wanted they told me they thought it was the wisest thing to do.'
Fears Remain for Many
Women who have cancer in one breast have a three- to fivefold higher risk of developing a second cancer in the opposite breast, and the risk is even higher among women with a family history of the disease.
Studies suggest that the removal of one or both breasts can reduce future breast cancer risk by about 90%, according to the National Cancer Institute.
In the newly published study, 519 women who had a disease-free breast removed while being treated for breast cancer were surveyed along with 61 breast cancer surviv"
more info at:
www.dreddyclinic.com
Subscribe to:
Posts (Atom)



